Often we end up striving for perfection where excellence will do. Neurosurgeons learn this eventually on the operating table.
We were operating on a ruptured intracranial aneurysm in the middle of the night. In such an operation, the intention is to place a clip on a 9 mm aneurysm, which, in effect, secures it from re-bleeding. While doing so, one has to ensure that the parent vessel from which the aneurysm arises is not compromised. To witness the astounding anatomy of the brain under a microscope at anytime of the day is special, but at 1 AM, there is something rivetingly enchanting about it. The obstreperous buzz of the operating room is doused at night. There are fewer people. Exits and entrances are less dramatic. You talk softer, you communicate less, and you can even hear your assistant breathe.
We neatly dissected silvery strands off the blood vessel and identified our target. I took a slightly curved titanium clip, and in a gentle, nimble move, opened its fangs and placed it gingerly along the entire length of the neck. This is the operation. That’s it. We were done. I then carefully inspected the anatomy with an endoscope to get a 360-degree view, to ensure there was no remnant hiding opaquely out of sight. Unfortunately, about 2 mm of the neck still lay unclipped.
“We have to advance the clip a little,” I decreed. “Leave it, sir, it’ll thrombose eventually ,”proposed my assistant, who usually believes in my sagacity more than I do. After all, everyone desires a good night’s sleep. When I was a resident in training, I remember coaxing my boss that the operation was “superbly performed” so that he would leave and allow me to close quickly, such that I could catch a few winks of much-needed slumber before the brightness of the next day loomed over us.
“Neurosurgery is a precision sport. It demands exactness,” I lectured now, succinctly, at 2 AM, as I advanced the clip to be perfect. As I withdrew my hand, the clip applicator failed to disengage from the clip and I ripped the parent artery in the bargain. In 3 seconds, the brain was full of blood. From cruising on an empty highway, we were suddenly in the middle of a massive pile-up. Alarms jarred, the ECG on the monitor convulsed, and we got in an extra suction to clear the blood and another nurse to scrub.
William Halstead once said, ‘the only weapon an unconscious patient has against an incompetent surgeon is haemorrhage.’ But we had a capable team.
After a few minutes of the catastrophe, I was able to locate the bleeding point and stop it by suturing the wall, but I had narrowed its calibre in the bargain. We had to perform a rescue bypass to augment the flow to the normal brain to ensure that he didn’t have a stroke later. I finally removed my gloves at 7 AM, when just a few hours earlier, I had visualised myself lying peacefully in bed long before then.
After every single surgery, no matter the time and how effortless or torturous it may have been, I sit in solitude for a few minutes to carry out an in-depth analysis in my mind of every step of the operation from opening to closure. I close my eyes and play out every move, lingering over the manoeuvres that are more frangible. If there is a complication, I always debate between having pushed the envelope too much and erring on the side of safety. As surgeons, we strive for this perplexing balance every day. In this case, did I do what was best for this patient in my hands? Was it really necessary to adjust the clip, or in the wise words of John Lennon, should I simply have “let it be”? If the applicator hadn’t gotten stuck to the clip, we would have been done in a few extra seconds, but it did and it ruined our night. Luckily, the patient recovered swiftly and was discharged after a slightly prolonged hospital stay.
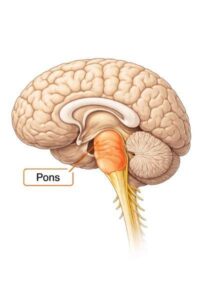
A few months later, we were removing a tumour from the insula, a small region of the brain buried between the frontal and temporal lobes. The deepest portion of the tumour was abutting the area that controls the movement of the left arm and leg. After having removed most of it, we kept resecting the tumour at the depth guided by the neuro-monitoring signals that alert us if we are causing any potential harm. My intuition signalled me to stop but the normal signal feedback we got was cushioning my gut. The more of the tumour that you remove, the better is patient survival, and so we removed it to the extent dictated. But the patient woke up paralysed on the left side. In those moments of solitude after every surgery, cloistered in the confines of an operating room corner, you sometimes need to ask for forgiveness (from the patient and their family) and hope that what makes your heart ache now will ache a little less later. However, as one of my favourite writers Cheryl Strayed says, “Forgiveness doesn’t sit there like a pretty boy in a bar. Forgiveness is the old fat guy you have to haul up a hill.” And every surgeon has a mountain to climb after every major error, no matter how inadvertent.
Not long ago, I was operating on a patient with a large lumbar disc herniation, a facile surgery done by me a few times a week. I decompressed the root diligently, but as the disc was calcified and causing compression on the other side, I tried to decompress it a little more so that he wouldn’t face problems in the future with the opposite leg. In the process, it led to a rent in the dural tube from which spinal fluid leaked out and nerve roots started popping out like spaghetti in a clear soup. We spent the rest of the day repairing the rent. The patient healed well but I ended up ageing quite a bit.
Too often, we strive for perfection where excellence will do. Most neurosurgeons obsess about the nitty-gritty’s of everything. The way we do one thing is the way we do everything. While this may seem great on the surface, it has the potential to harm at the depth. With this attitude, it is possible that we might hurt our patients, do a disservice to our personal relationships, and battle with our own peace. Over the years, therefore, I’ve come to soften my stance on perfection by transforming it as Maya Angelou suggests: “Do the best you can until you know better. Then when you know better, do better.”




0 thoughts on “The Perfect Storm”
We stumbled over here different page and thought I may as well check things out. I like what I see so i am just following you. Look forward to checking out your web page yet again.
dance shoes that are shiny are the most cool stuff that you could possibly wear**