Training a young medical student from Germany, a surgeon dips into the learnings from his formative years at the Grant Medical College to dole out important life lessons

I recently had a medical student intern with me for a few weeks. Rukin had finished two years of medical college in Germany, and as he was interested in neuroscience, he decided to shadow me during his vacation. He was a sharp, well-groomed boy with a deep husky voice and full crop of thick black hair – none of the qualities I had possessed as a medical student.
He was 21. I am 42. Looking at him, I couldn’t help but remember my time as a medical student. About a little more than two decades ago, I stood meekly outside the administrative office of Grant Medical College and Sir JJ Group of Hospitals, immensely grateful to have secured admission with a little bit of merit and a lot of luck. In 1999, ours was the first batch that discounted the HSC marks and had a separate medical entrance exam. I remember 200 of us gathered in the voluminous anatomy lecture hall, where pigeons used to routinely fly across the room during lectures. Our anatomy professor was a pleasing roundish gentleman with buck teeth that allowed the air to pass through smoothly every time he spoke. “Anatomy is something everyone has, but in my opinion, it looks better on a girl,” was his icebreaker, amidst a few giggles and many glares.
“Do you get to dissect dead bodies?” I asked Rukin, who was scrubbing in beside me on a case we were about to work on. “Yes, but not like you get them in India,” he confessed. “Here, whenever you need a body, it can be made available to us!” I joked, adding, “Let’s not jinx it for this patient today, though.” Nothing paralleled the thrill of dissecting a dead body allotted to you, I told him. At Grant’s, as it was fondly called, we had called our cadaver John and considered him to be British – because he was fair and had a stiff upper lip. The dissection hall in the department of anatomy was where the dead taught the living. It was also a place where we resuscitated our colleagues who fainted at certain sights, the smell of formalin making deep inroads into their gentile infrastructure. Over the course of one year, John taught us more than our textbooks did. It was also the only place where we washed our hands before going to the bathroom.
The surgery today was on someone’s cervical spine. “Go ahead and make the incision,” I said, handing over the knife to Rukin, who took the knife a little warily. I added, “Be careful – the carotid artery is right underneath it!” and he handed it right back to me. I didn’t know if I was inspiring someone to become a surgeon or deterring him from it.
While I operated, I told Rukin more about Grant Medical College. Nearly every famous doctor in the world, we claimed, was from this legendary institution. Some even went on to act in movies or became singers, business tycoons, and CEOs. We were given a well-rounded training very different from that given by other medical colleges, who only concentrated on education. I remember being awestruck back in the day when I learned that pioneering work on malaria was done at Grant’s, when a new blood group was discovered there. “Did you know that besides the regular A, B, AB, and O blood groups, there’s something called a Bombay blood group?” I asked him. He shook his head behind his mask. “Grant’s made this discovery!”
Waldemar Haffkine worked on and perfected the inoculation of the plague vaccine in the Framji Dinshaw Petit Laboratory of Grant Medical College, which then became the pharmacology lecture hall where we ended up snoozing in every class; little did we know that it was here that the foundation of the Haffkine Institute was laid. Robert Koch worked on cholera and TB in our labs. Henry Vandyke Carter discovered the pathology of spirochetes in relapsing fever on our premises. Even the founder dean of our rival college, KEM, trained at Grant’s. From a 2-room teaching hospital on an area of 4 acres, Grant Medical College and Sir JJ Group of Hospitals stand on 44 acres today, I reminisced proudly.
Back then, however, in our first year of medical school, different kinds of poignant and extremely significant discoveries were made: that the canteens had more items on the menu thanks to us, the boys’ common room was kept open beyond the permitted hours, the college festival lasted one week instead of the usual 4 days, and couples found newer places to express their love. Study leaves became longer but were utilized for everything but study. Teachers became friends and friends became teachers… but attendance continued to remain a problem. In all the fun and frolic, we continued to be aware of our responsibilities. We were focused and determined as we walked into hospital each day with a smile on our face and a song in our hearts, not forgetting to pay our respects to the robust statue of our founder, Sir Jamsetjee Jejeebhoy, and seek his blessings.
On his part, Rukin told me that it was becoming apparent to him how different his medical training was as compared to the one I had received. At his college, they are compelled to separate the theory from the practical aspects of medicine. Cadavers, for them, were supplementary sources of education that aren’t heavily emphasised, and he’d taken it upon himself to read MRI and CT scans on his own time, because he wanted to prioritise practicable knowledge over memorising textbooks.
“What kind of exams do you have in anatomy once you finish your first year?” I asked Rukin. “Two practical exams, one on models and one on a computerized cadaver, apart from the theory,” he explained. “In our scenario, everything is real,” I told him. “Real specimens, real cadavers!”
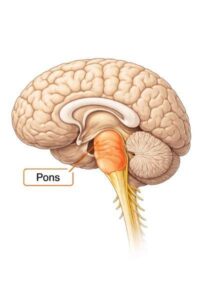
I vividly remember my first-year anatomy exam viva. One of the test questions was to identify a body organ that had been stored in a formalin jar for decades and talk about it for a few minutes. Out of a few dozen jars in the anatomy lab, the professor would place one on the table in front of us and ask us to speak at length. He was jovial but intimidating. Even if we couldn’t describe its anatomy in detail, he said, it was important that we identify the organ correctly to be able to pass. I was sitting on a stool 3 feet behind the boy whose turn it was before mine, and the examiner placed a shrivelled specimen of a uterus in front of him, which I could identify with ease even from a distance. The examinee was having a hard time figuring it out, however; he turned the jar in all directions to decipher what it could be and the ashen look on his face revealed he was clueless. “I’ll give you a hint,” the professor prodded with a smile. “It’s something you and I don’t have.” With a slight sense of relief, he composed himself and gave it a shot. To his own disbelief and that of everyone else in the room, he answered, “Brain?” Needless to say, he was asked to re-appear for the exam six months later.
At the end of his internship, Rukin left us feeling both elated and a little melancholy: elated because he couldn’t picture himself not being a surgeon in the future, and melancholy because he realised he wouldn’t be able to be inside an OR for a long while. In his own words, “You gave me a sense of belonging and something to really look forward to at the end of my studies. I didn’t want to be a surgeon because of the pressure originally, but you let me discover something that I truly love, and I am not scared anymore.



0 thoughts on “The Surgical Intern”
Кредит под залог: ваши финансовые возможности, новые возможности.
кредит под залог квартиры без дохода [url=https://www.ctekc.ru/]https://www.ctekc.ru/[/url] .